

Acknowledgment I am greatly indebted to the expert editorial and administrative assistance of Kathy Mandery for the preparation of the manuscript for this chapter. Risk of dementia in peritoneal dialysis patients compared with hemodialysis patients. Gene alterations in complement proteins have been shown to predispose persons to the development of hemolytic uremic syndrome. Theoretical concerns regarding the inability of the failing liver to metabolize citrate appear to be not borne out by recent clinical experience. Phenylephrine is a pure vasoconstrictor and is not recommended for empiric use, although niche uses for phenylephrine include (1) difficulty raising mean arterial pressure in the presence of high cardiac output as well as (2) serious tachyarrhythmias induced by norepinephrine (not usually an issue). Protocolized or not, resuscitation from septic shock remains principally crystalloid based in sharp contradistinction to hemostatic resuscitation for those presenting in hemorrhagic shock after injury. This difference demonstrates the significant effect of secondary membrane formation on membrane function. Consequently, in dialysis using cellulose acetate membranes, complement activation is attenuated, as is the leukopenic response, in comparison with dialysis using unmodified cellulosic membranes. The renal volume increases by as much as 30%, and the overall dimensions of the kidney increase by approximately 1 cm. Because the kidneys are in the retroperitoneal space, unlike other viscera, there is lesser tolerance for organ expansion in the setting or organ edema. Epidemiological approach to identifying genetic predispositions for atypical hemolytic uremic syndrome. Indeed, allantoin is 5- to 10-fold more soluble than uric acid and is excreted readily. Efferocytosis is the phagocytosis of apoptotic neutrophils and cellular debris primarily by macrophages, whereupon they are clear the tissues and migrate to regional lymphatics for disposal. However, a recent retrospective cohort study has suggested an association with 2-year graft survival (but not with early graft function or decreased rejection episodes). Protective effects of curcumin on acute gentamicin-induced nephrotoxicity in rats. Plasma potassium in patients with terminal renal failure during and after haemodialysis; relationship with dialytic potassium removal and total body potassium. Conventional hemodialysis remains an important renal replacement modality for critically ill patients with acute kidney injury. Serum and urinary neutrophil gelatinase-associated lipocalin levels in children with chronic renal diseases. Late-onset renal failure after liver transplantation: role of posttransplant alcohol use. A recent consensus statement proposes that congestion be graded according to a combination of clinical and laboratory parameters (Table 119. Surviving sepsis campaign: international guielines for management of severe sepsis and septic shock: 2012. The microcrimped polysulfone fibers contained in the dialyzers used in this study have a relatively low amplitude and high frequency. This fluid removal rate may be inadequate for some patients, as suggested by the lack of difference in weight loss between the two groups at the 96-hour assessment. Glycocalyx disruption resulting from sepsis and cytokines contributes to increased permeability, in systemic and renal microcirculation, increasing leukostasis, microthrombosis, fluid shift, and interstitial edema. Urea kinetics during sustained low-efficiency dialysis in critically ill patients requiring renal replacement therapy. In the absence of diuretic responsiveness, techniques available for fluid removal are ultrafiltration, hemofiltration, hemodialysis, and hemodiafiltration. Multicenter clinical evaluation of the HeartMate vented electric left ventricular assist system in patients awaiting heart transplantation. Attention must be paid to the position of the patient and fixation of the catheter to prevent kinking at the site of insertion. They reported that improvement in the level of consciousness was achieved in 33 (70. Particularly during "normal" seasonal influenza years, there is significant local variation in the onset and termination of the flu season. The available data on various types of treatment have been taken into consideration in the position papers issued by the medical societies. One study of intensive care unit patients undergoing continuous invasive monitoring showed a moderate correlation (r = -0.
For intermittent therapies, because of the high blood flow requirements needed, hemofiltration is technically more demanding and may best be coupled with a degree of diffusive clearance (intermittent hemodiafiltration). These alterations occur early in gestation, even preceding the early gestational changes in plasma volume and cardiac output, thereby anticipating the future needs of the growing fetoplacental unit. Combination of extracorporeal membrane oxygenation and continuous renal replacement therapy in critically ill patients: a systematic review. These decrements are approximately 32% and 24%, respectively, from normal late-pregnancy levels. For example, in the largest randomized controlled trial in kidney donors conducted by Kainz et al. Pharmacokinetics and pharmacodynamics of mineralocorticoid blocking agents and their effects on potassium homeostasis. Intrathoracic, intrapulmonary, and intra-abdominal pressures increase during inspiration and remain positive during the breathing cycle. The electrolytes are present in the plasma water only, and the body is responding to that. Activated charcoal adsorbs many substances such as alkaloids, vitamin K antagonist, and acetaminophen, but many other kinds are not adsorbed. The patient receiving parenteral nutrition has no protective mechanism for dealing with overfeeding and must assimilate substrate. Some interventions are alluded to only briefly because they are addressed in detail in other chapters; for further information, the reader is directed to those chapters. Therefore significant anasarca may impair intestinal absorption via mucosal edema. Demonstrable beneficial effects of eplerenone in patients with cardiac failure after myocardial infarction are similar to those of spironolactone, including significantly better mortality and hospitalization outcomes. Discuss the available evidence to guide the use of loop and thiazide diuretics in the acutely ill patient. A multicenter pilot randomized controlled trial of remote ischemic preconditioning in major vascular surgery. Still, other conditions may additionally aggravate thrombocytopenia through either platelet consumption or reduced production; these include sepsis, viral infections, hematinic deficiency, disseminated intravascular coagulation, cirrhosis, autoimmune diseases, adverse reactions to drugs, and thrombotic microangiopathies. In this study of 145 treatments, there was a drop in average serum phosphate concentration from 5. A clinically sound and compassionately administered medical approach should be considered good and adequate unless refused by the patient. Electrolyte shifts across the artificial lung in patients on extracorporeal membrane 14. Peritoneal dialysis fluids are relatively hyponatremic, and patients may require additional hypertonic sodium infusions to maintain a high plasma sodium concentration. Viruses are a common cause of critical illness and should be evaluated to facilitate de-escalation of other therapies. Explain the negative effects of extra cellular fluid volume expansion on cardiac and renal function. The drugs that are most efficiently removed by renal replacement therapies are those with low volume of distribution, low protein binding, and high renal clearance; this is the case for most hydrophilic antibiotics belonging to the classes of lactams and aminoglycosides. Discuss the association between metabolic acid type and outcome in critically ill patients. The pathogenesis of nephropathia epidemica: new knowledge and unanswered questions. The relationship between dialysate magnesium concentration and bone disorders in patients undergoing hemodialysis is complex and requires further study for clarification. Fractional excretion of urea as a diagnostic index in acute kidney injury in intensive care patients. Results of these studies23,24 align with a recent single-center study from France25 and clearly position the use of heparin-grafted membranes as a valid alternative to saline infusion in patients at high risk of bleeding. Sustained low efficiency dialysis using a single-pass batch system in acute kidney injury-a randomized interventional trial: the renal replacement therapy study in intensive care unit patients. Examine the causes of venous and arterial thrombosis in uremia and acute renal failure. Excerpts from the United States Renal Data System 2004 annual data report: atlas of end-stage renal disease in the United States.
The evaluation of effects of demographic features, biochemical parameters, and cytokines on clinical outcomes in patients with acute renal failure. Biomarkers in cardiovascular disease: integrating pathophysiology into clinical practice. Systemic use of compstatin would require reliable dose-responses and a wide margin of safety for the drug. Sustained low-efficiency daily diafiltration for diabetic nephropathy patients with acute kidney injury. If the patient loses residual renal function, then more frequent dialysis must be provided. Ascitic fluid should be inoculated at the bedside, using blood culture bottles, including aerobic and anaerobic media. In both settings, divalent cations of Mg and Ca are present, with the possibility of carbonate precipitation. Role of Kidney Hypoxia the final common pathway of the pathophysiologic response to sepsis, as discussed above, leads to tissue hypoxia. Analysis of a urinary biomarker panel for clinical outcomes assessment in cirrhosis. Its duration can be prolonged in poisoning patients depending on the clinical context. When this occurs, this is a poor prognostic sign indicating that systems that work to maintain the plasma concentration of sodium near 140 mEq/L have failed and that short-term cardiac compensation, as well as some degree of brain edema, is imminent. The choice of antibiotic coverage should be governed by the organisms involved, based on either epidemiologic data or documented culture results. Intensive hemodialysis associates with improved pregnancy outcomes: A Canadian and United States cohort comparison. Conversely, larger molecules, which have a lower sieving coefficient, are trapped and washed out. Obviously, the competent patient can change his or her position; in this sense, informed consent is a continuous process and not a single event. Heparin may be administered as an intermittent bolus or as a continuous infusion through a dedicated syringe pump (in the machine or external) that allows highly accurate control of the volume infused. Actually, such supports tend to be self-justifying for the mere reason that they are at least temporarily lifesaving. Prognostic significance of blood lactate and lactate clearance in trauma patients. These are all acute phase proteins from the liver that are expressed in acute inflammatory states. Cellular therapies aim to use cells that are capable of modulating the global inflammatory response by secreting large quantities of proinflammatory and antiinflammatory agents and other types of molecules. The therapeutic options in treating these resistant gram-negative organisms include carbapenem, tigecycline, high-dose ampicillin-sulbactam, colistin, fluoroquinolone, aminoglycosides, ceftaroline, ceftazidimeavibactam, ceftolozane-tazobactam, and fosfomycin. Urinaryneutrophil gelatinase-associated lipocalin as biomarker in the differential diagnosis of impairment of kidney function in cirrhosis. Investigation of a Rise in Obstetric Acute Renal Failure in the United States, 1999-2011. Impact of Platelets and Platelet-Derived Microparticles on Hypercoagulability Following Burn Injury. Components of energy expenditure in patients with severe sepsis and major trauma: A basis for clinical care. Worsening renal function and prognosis in heart failure: systematic review and meta-analysis. Proteinbound substances bind to the adsorptive material in the column and are removed from circulation. Clinical review: the meaning of acid-base abnormalities in the intensive care unit-epidemiology. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: A multiple-center epidemiological study. For a given solute, diffusive mass transfer resistance in the blood compartment of a dialyzer is the ratio of effective diffusive path length (x) to effective solute diffusivity (D), both of which may be influenced by hematocrit. Cascade filtration is a semiselective technique that minimizes the use of replacement fluids while efficiently removing circulating antibodies. Volume resuscitation to ensure optimum hemodynamic support and adequate urine output (3 L/day) are of critical importance in the initial management.

Omega-3 Fatty Acids There have now been two recent studies79,80 in which enteral nutrition products containing fish oil (eicosapentaenoic acid), borage oil (gamma-linolenic acid), and antioxidants led to beneficial clinical outcomes in patients with acute lung injury and septic shock. However, there was a wide heterogeneity in the definition of nephrotoxicity across trials. Unfortunately, information to the patient is often inadequate, and advance care planning and advance directives are rare in everyday clinical practice. In the 1960s, soon after the beginning of use of hemodialysis in patients with chronic renal failure, attempts were made to shorten the duration of each treatment as a means of cost reduction and to satisfy patients who naturally prefer short versus long treatment sessions. Most complications occur because of nonspecific adsorption of biologic components to the column. The rotational speed of the pump depends on the blood flow prescription and is proportional to the stroke volume, defined by the geometry of the pump and the inner diameter of the blood tubing. The expert consensus suggested that a congestion grade of more than 12 together with low urine output (<1000 mL/24 hr) should trigger the use of extracorporeal a fluid removal because, in patients with this degree of congestion, diuretics are less likely to effectively reduce fluid overload. Lactate is crucial for intercellular and interorgan cooperation, substrate distribution, and perhaps adaptation to injury, and thus hyperlactatemia cannot be an exclusive reflection of tissue hypoxia. Beyond plasma exchange, fresh frozen plasma infusions and corticosteroids often are used when severe symptoms supervene or clinical improvement is lacking after withdrawal of the offending drug; the utility and timing of these additional measures is not clear. Crystalloid solutions should be used for volume expansion if needed rather than colloid solution. The addition of chelating agents, pre- (and possibly post-) treatment, can improve total clearance through dialysis, filtration, or adsorption of the metal-chelator complex. Biochemical effects of phosphate-containing replacement fluid for continuous venovenous hemofiltration. A fatal case of poisoning by lidocaine overdosage-analysis of lidocaine in formalin-fixed tissues: A case report. Vasopressin deficiency and pressor hypersensitivity in hemodynamically unstable organ donors. Continuous blood volume assessment indicates the need to slow ultrafiltration rates to reduce marked changes in blood volume. Moderate to severe cognitive impairment occurs in 30% to 60% of patients undergoing hemodialysis,12 and two thirds of patients undergoing peritoneal dialysis. Glucose dynamics during continuous hemodiafiltration and total parenteral nutrition. Albeit generally reversible, AmB-induced kidney injury is not a benign complication. The primary goal is to secure the circulating volume and to maintain the water and electrolyte distribution. To estimate the total plasma concentration of an electrolyte, the first step is to convert the measured activity to the concentration in plasma water. Therefore, despite its clinical importance, the increase in H+ is negligible from a quantitative point of view. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of Compartment Syndrome. Prevalence and patterns of renal involvement in imaging of malignant lymphoproliferative diseases. However, meta-analyses suggest excess mortality with Cuprophan membranes, at the limit of significance. Albumin dialysis with a noncell artificial liver support device in patients with acute liver failure. Increased Fluid Administration After Early Acute Kidney Injury is Associated with Less Renal Recovery. Furthermore, the watersoluble contrast is taken up readily by the apical surface of proximal tubular cells (pumps, bystander endocytosis) and out the basal-lateral surface into the tubule interstitial space. Also, by explaining buffering, we examine the connections between the proton-focused discourse and the chargebalance paradigm to show that some of the disagreements are mainly apparent because strong ions are implicated in both discourses. Treatment of acute carbamazepine intoxication according to its pharmacological properties. Importantly, insufficient activation of mitophagy has been associated with a worse outcome in critically ill patients and has been postulated to contribute to cell and organ dysfunction.

Plasma brain natriuretic peptide concentration on assessment of hydration status in hemodialysis patient. This eight amino acid oligopeptide has many physiologic effects, which include stimulation of central neural centers associated with increased thirst and heightened activity of ganglionic nerves via its effects on the autonomic nervous system. The dose and patient response in the critically ill are variable, and antibodies to heparin can make this method ineffective. A soft-tunneled dual-lumen catheter (or dual catheter) is indicated in a patient with acute renal failure when renal replacement therapy is expected to exceed 2 weeks, to prevent complications. This results in a higher-than-usual fraction of the drug reaching the intended receptors and may be manifested in more toxicity than expected. Effective hypovolemia is caused by a splanchnic arterial vasodilation and a reduction in cardiac output. In the latter situation, diffusion and convection interact in such a manner that total solute removal is significantly less than what is expected if the individual components are simply added together. On the contrary, fluid liberal protocols may induce various degrees of overhydration with consequent peripheral and pulmonary edema, congestion, and renal dysfunction. The first objective was to arrive at a task force consensus on a few clinical measures that have face validity as proxies for circulatory and cellular/metabolic abnormalities. Larger prospective validation across multiple centers, which includes a comparison of the devices used, is necessary before such criteria can be accepted widely as a standard of care. Subarachnoid hemorrhage is more common in patients with malignant hypertension and in those with polycystic kidney disease. Because a limited number of donor hearts are available in the United States each year for transplantation, the need for other approaches to cardiac replacement is now well established. Development of severe hyponatraemia in hospitalized patients: treatment-related risk factors and inadequate management. They can include a "living will" (an instruction directive in which the patient specifies the level of acceptable therapy) and/or a proxy directive ("durable power of attorney for healthcare," in which the patient indicates the person who can make sound decisions in her or his place, should she or he become incompetent). These investigators found better hemodynamic stability with continuous therapy despite a significant increase in net fluid loss during 3 days (cumulative median value), -4 L versus +1. Transition from left ventricular hypertrophy to massive fibrosis in the cardiac variant of Fabry disease. Conversely, clearance can be increased with volume expansion, loop diuretics, and interruption of distal sodium (and lithium) reabsorption with amiloride or triamterene. Patients may experience stabilization and de-escalation and then move back to the rescue or optimization phases because of a new clinical event,19 and many hospitalized patients will not require fluid boluses. These may include an anesthesia-induced decrease in effective blood volume, preexisting cardiovascular disease or severe cardiomyopathy, prolonged episode of hemodynamic instability or hypotension, severe intravascular volume depletion, use of drugs that can adversely affect intrarenal hemodynamics, older age, preexisting renal dysfunction, and diabetes mellitus. Increased aerobic glycolysis thus results in the increased production of lactate, which is independent of oxygenation. Continuous glucose measurements may assist in achieving less variability (higher quality) of blood glucose control in critically ill patients. In the lung and kidney this results in necrosis, hemorrhage, and loss of effective glomerular filtration and pulmonary gas exchange, causing the clinical syndromes of respiratory failure and oliguric kidney failure. Hypotension is a complication that can occur when the rate of removal of plasma water exceeds the refilling capacity. Subcutaneous endoscopic fasciotomy in a porcine model of abdominal compartment syndrome: A feasibility study. Nevertheless, renal function on postoperative day 7 and the need for hemodialysis/hemofiltration during the first week were similar in both groups. Mechanisms of renal vasodilation and hyperfiltration during pregnancy: current perspectives and potential implications for preeclampsia. Theory before practical, simple to complex, abstract to concrete is the best advice. In addition, the term hepatorenal disorders was proposed to encompass the full range of conditions in which liver and kidney disease coexist.
Duboisia myoporoides (Corkwood Tree). Probenecid.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96470
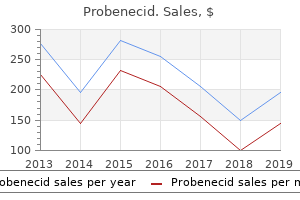
High-Dose Versus ConventionalDose Continuous Venovenous Hemodiafiltration and Patient and Kidney Survival and Cytokine Removal in Sepsis-Associated Acute Kidney Injury: A Randomized Controlled Trial. Clinical Implications of Intrarenal Hemodynamic Evaluation by Doppler Ultrasonography in Heart Failure. Since that time, individualizing dialysate content for particular patient needs and maintaining water purity have been major fields of interest in dialysis practice. The timing of renal replacement therapy initiation in acute kidney injury: is earlier truly better Fluid balance and urine volume are independent predictors of mortality in acute kidney injury. Metformin is an antidiabetic drug that can result in lactic acid accumulation and worsen heart function because of a negative inotropic effect. Nonelevated serum levels of these two enzymes often suggest that the diagnosis of pancreatitis is less likely. Effect of membrane composition and structure on performance and biocompatibility in hemodialysis. Acidosis, also a prominent feature of acute renal failure, promotes potassium exit from the cells. Nitrogen is lost in body secretions and excreted in sweat, feces, and urine, the latter most notably as urea nitrogen that accounts for 85% to 90% of urinary nitrogen loss. Peritoneal fluid generally has a zero potassium bath, so exchange should be conducted roughly on an hourly basis for life-threatening hyperkalemia. The role of cytokines in mediating acute hypotensive and febrile reactions as well as metabolic, immunological and inflammatory changes was first introduced by Henderson and colleagues as "the interleukin hypothesis"29. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. Explain how endothelium damage translates into a loss of kidney function: sepsis-induced acute kidney injury. Data analytics for continuous renal replacement therapy: Historical limitations and recent technology advances. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomized non-inferiority trial. A low serum total magnesium concentration may well represent pseudohypomagnesemia in a severely hypoalbuminemic patient. Aldosterone has a powerful effect on the principal cells in the collecting ducts to reabsorb sodium, provided there is adequate delivery of urinary sodium to the distal nephron, as well as release potassium into the urine. Unfortunately, these agents reportedly proved to be useful only within small case series of just single case reports. However, there is a considerable amount of ongoing and completed animal research that points to an improved surrogate and clinical outcomes, including in disease processes such as ischemia-reperfusion injury,30 sepsis,31 toxic injury,23,32 and obstructive aeropathy. Urinary strong ion difference is a major determinant of plasma chloride concentration changes in postoperative patients. Prerenal azotemia: differentiation of hyperureagenesis from renal hypoperfusion using urinary urea nitrogen data. As an alternative or first choice, heparin is administered into the circuit blood pathway before the membrane and is dosed to elevate the activated clotting time to a level close to or within therapeutic range for the local hospital lab. With regard to treatment session length, many machines in North America can perform treatments for 24 hours or even continuously. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. High-dose intravenous selenium does not improve clinical outcomes in the critically ill: a systematic review and meta-analysis. Pathophysiology of the upper gastrointestinal tract in the critically ill patient: rationale for the therapeutic benefits of acid suppression.
Syndromes
At filtration fractions beyond this value, hemoconcentration is associated with an environment that promotes interactions between formed elements and proteins in the blood and the filter membrane, leading to a high risk of filter resulting from widespread pore occlusion ("clogging"). However, a more rigorous classification incorporating solute and water permeability properties has been proposed recently. Kidney function and mortality among patients with left ventricular systolic dysfunction. Oxygen and nutrients are shunted to the central nervous system and the stressed body sites where they are most needed. It is influenced by renal injury as well as the less common hyperfunctioning kidney. The sympathetic nervous system in heart failure physiology, pathophysiology, and clinical implications. Basically, urinary phosphate excretion reflects dietary phosphate intake (Table 58. The two components (bicarbonate and calcium-containing) then are combined in a given proportion by the dialysis machine, offering a wide range of final bicarbonate concentrations depending on the clinical situation. Artifactual elevation of measured plasma L-lactate concentration in the presence of glycolate. Adenosine diphosphate in red cells as a factor in the adhesiveness of human blood platelets. Matching energy requirement to energy expenditure may not be optimal for nutritional management. Another relatively recent development is the incorporation of polysulfone-based membranes having mean pore sizes that are substantially typical infusion rate (at least 1 L/hr) required to achieve the desired anticoagulant effect augments the total fluid volume (blood plus anticoagulant solution) delivered to the blood pump. Metabolic acidosis, as well as metformin plasma concentrations, were reduced dramatically in the first 24 hours and/or normalized on the second day in every case with no rebound in acidosis. Complications may be classified generally into two broad categories, clinical and technical. Indeed, as mentioned above, chronic use of loop diuretics leads to distal tubule hypertrophy. Treatment is targeted at decreasing the production of the amyloidogenic light chain. However these findings were not confirmed by other studies and need to be further investigated59,60. Several lines of evidence indicate that increased levels of proinflammatory cytokines may explain the hypocholesterolemia of acute illness. These variables are assessed in their own right and are used to derive other variables, such as tonicity, water balance, anion gap, strong ion difference, and strong ion gap. Effect of enteral feeding with eicosapentaenoic acid, gamma-linolenic acid, and antioxidants in patients with acute respiratory distress syndrome. Likewise, sepsis nonsurvivors show significantly lower expression levels of genes involved in antigen presentation and T cell function when compared with survivors. Choice of renal replacement therapy modality and dialysis dependence after acute kidney injury: a systematic review and metaanalysis. An ultrafiltration control system is required to prevent excessive ultrafiltration. Meanwhile, certain "standard" dialysate prescriptions are offered in most centers and serve as the starting point for adjustments to meet patient needs. Stomatitis and glossitis, often accompanied by a dry burning mouth, commonly are associated with poor dental hygiene. Examine the consequences of technical modifications to continuous renal replacement therapy. Enterovirus and West Nile virus, in particular, have a predilection for this aftereffect. Although predicted effects mediated through renal mechanisms include improved blood pressure control and resolution of edema, significant natriuresis is not achieved universally.

Characteristics and Outcomes of Granulomatosis With Polyangiitis (Wegener) and Microscopic Polyangiitis Requiring Renal Replacement Therapy: Results From the European Renal Association-European Dialysis and Transplant Association Registry. Position statement and practice guidelines on the use of multidose activated charcoal in the treatment of acute poisoning. The compensatory activation of endogenous vasoconstrictors systems such as sympathetic nervous system, the renin-angiotensin-aldosterone system, and nonosmotic secretion of vasopressin leads to severe prerenal arterial vasoconstriction. Slow hemodialysis performed during the day in managing renal failure in critically ill patients. Hypernatremia is less common than hyponatremia, but the patient is generally more ill and has a higher mortality according to large retrospective studies. A randomized, controlled, multicenter trial of the effects of antithrombin on disseminated intravascular coagulation in patients with sepsis. These patients will present with hyperchloremic metabolic acidosis with a normal serum anion gap. No difference in myocardial infarct size (defined by elevated high-sensitivity troponin T and myocardial perfusion scintigraphy) was found. Such barriers can be overcome through paired exchange programs or desensitization strategies. In consideration of the very high mortality in an end-stage organ failure, these supportive therapies represent a significant advance in medical technology and techniques to prolong survival. One-year survival estimates were 52% in the device group versus 25% in the medical management group and at 2 years, the survival in device group was 23% as opposed to 8% in medically managed patients. All of these mechanisms contribute to the microvascular dysfunction phenotype characteristic of sepsis to further oxidative stress and inflammation. Septic acute kidney injury in critically ill patients - a single-center study on its incidence, clinical characteristics, and outcome predictors. Urine sodium profile in the course of septic acute kidney injury: insights relevant for kidney function monitoring. A consequence of this gastric hyperpermeability is an augmented back-diffusion of hydrogen ions from the gastric lumen to the mucosa. Congestive heart failure, cirrhosis, and nephrotic syndrome are complicated frequently by hypervolemic hyponatremia. Straight or kinked double-lumen catheters exiting in an unfavorable area (middle or upper neck) are uncomfortable, difficult to fix, protected by dressing, and more exposed to infections. Therefore it is obvious that more effective and specific treatment options are needed urgently to improve outcomes. Arginine vasopressin significantly increases the rate of successful organ procurement in potential donors. Liver transplant may be required in rare cases of severe and persistent liver dysfunction. Greaves M, Control of Anticoagulation Subcommittee of the S, Standardization Committee of the International Society of T, Haemostasis. Nitric oxide induced contractile dysfunction is related to a reduction in myocardial energy generation. The ingested amount of ethylene glycol required to produce toxicity in animals is approximately 1 to 1. Nevertheless, despite playing a crucial role in metabolic acid-base disturbances, it does not contribute in buffering respiratory acid-base disorders. In this setting, the bioreactor consists of hepatocytes that are cultured in a three-dimensional extracellular matrix and surrounded by a hollow-fiber capillary system to allow plasma perfusion. Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. It is well known that the cognitive function was improved after the completion of a dialysis session.
Anatomic alterations of sarcomere muscle tissue resulting from posttranslational modifications of titin (a protein that connects the Z-line to the M-line in the sarcomere) are responsible for increased stiffness. Continuous treatment is suggested to deliver a urea clearance of at least 2 L/hr, with the clinical evidence that 20 to 25 mL/kg/hr may be the best prescription. These two pathways activate factor X, leading to thrombin formation, followed by the conversion of fibrinogen to fibrin. Modification of Acid-Base Balance in Cirrhotic Patients Undergoing Liver Resection for Hepatocellular Carcinoma. Artificial and bioartificial support systems for acute and acute-on-chronic liver failure. The velocity that blood achieves while passing through an individual hollow fiber membrane is directly proportional to its blood flow rate. Discuss the management of hepatorenal syndrome in the setting of spontaneous bacterial peritonitis. Cyproheptadine currently is recommended, although its efficacy has not been established rigorously. Induction therapy for patients with small-vessel vasculitis and rapidly progressive glomerulonephritis, pulmonary hemorrhage, inflammatory tracheal stenosis, and other serious manifestations is high-dose corticosteroids and cyclophosphamide. Physostigmine is an acetylcholinesterase inhibitor and, unlike neostigmine, crosses the blood-brain barrier. Although the modulation of inflammatory mediators appears to be the major objective of blood purification in sepsis, this therapy also may offer additional physiologic benefits, including temperature control, acid-base control, fluid balance control, cardiac support, protective lung support, brain protection, bone marrow protection, and blood detoxification and liver support. In that study the authors identified a group of patients who met acute kidney injury criteria after adjustment of creatinine for fluid balance (but not before). However, this agent should be used cautiously in patients who have congestive heart failure or who are taking beta blockers, digoxin, or a non-dihydropyridine calcium channel blocker. Other causes of death include cerebrovascular accidents (46%), sepsis (17%), multiple organ dysfunction syndrome (7. In hemodialysis, the mass removal rate of small solutes such as urea is very high during the early stage of an intermittent hemodialysis treatment, owing to a favorable transmembrane concentration gradient for diffusion at this time. Although the effective molecular weight cutoff is much lower after blood exposure, relatively substantial albumin loss (as much as 30 g per treatment) still occurs with use of these membranes. Use of online blood volume and blood temperature monitoring during haemodialysis in critically ill patients with acute kidney injury: a singlecentre randomized controlled trial. Residuals from this compound can cause lethal complications through lung embolism and exposure to hydrogen fluoride, a highly toxic decomposition product that can be generated using either and sterilization57. Hypertonic saline, not mannitol, should be considered gold-standard medical therapy for intracranial hypertension. Importantly, ultrafiltration can be controlled more tightly than the use of diuretics. Simple and accurate quantification of dialysis in acute renal failure patients during either the urea non-steady state or treatment with irregular or continuous schedules. Renal replacement therapy in critically Ill patients receiving extracorporeal membrane oxygenation. A double-lumen semirigid polyurethane catheter is the best catheter for starting the dialysis. Impact of duration of critical illness on the adrenal glands of human intensive care patients. Clinical review: Volume of fluid resuscitation and the incidence of acute kidney injury - a systematic review. Furosemide is by far the most used loop diuretic, evidenced by the fact that it is the only loop diuretic that figured among the top 20 most prescribed drugs in the United States in 2008,11 which was confirmed in a recent survey among intensivists. A novel attribute of enoxaparin: inhibition of monocyte adhesion to endothelial cells by a mechanism involving cell adhesion molecules. Neutrophil gelatinaseassociated lipocalin in the diagnosis of type 1 cardio-renal syndrome in the general ward. In this setting the increased lactate concentration likely serves as an important source of energy for vital organs (heart and brain). Glomerulonephritis is a rare cause of acute renal failure, especially in the intensive care unit, and may be misdiagnosed as acute tubular necrosis. Further, in the setting of immunosuppression, antibodies may not form for seroconversion, thus nucleic acid testing should be used to assess for infection. Carbon dioxide has also an effect on pulmonary vascular resistance, although controversial results have been reported.